- Silent Reflux is a condition where stomach acid flows up into the throat without causing heartburn.
- Choosing alkaline and low-acid foods can soothe the throat and reduce irritation.
- A reflux-friendly diet includes whole grains, lean proteins, and soothing herbal teas for symptom relief.
 Silent reflux, also known as laryngopharyngeal reflux (LPR), is a condition in which stomach acid flows back into the throat and voice box without the classic symptoms of heartburn, making it harder to detect and diagnose. Living with silent reflux often means managing subtle but persistent symptoms like hoarseness, chronic cough, throat clearing, and the sensation of a lump in the throat. Unlike gastroesophageal reflux disease (GERD), silent reflux doesn’t typically cause heartburn, but it can still inflict damage on the upper airway. Dietary changes are a cornerstone of treatment for this condition, as certain foods can aggravate or soothe the upper digestive tract. Studies emphasize that low-acid, anti-inflammatory, and alkaline-rich foods can reduce irritation and promote healing of the laryngopharyngeal area. Moreover, a tailored reflux diet helps to reduce the frequency of reflux episodes and improve quality of life for patients.
Silent reflux, also known as laryngopharyngeal reflux (LPR), is a condition in which stomach acid flows back into the throat and voice box without the classic symptoms of heartburn, making it harder to detect and diagnose. Living with silent reflux often means managing subtle but persistent symptoms like hoarseness, chronic cough, throat clearing, and the sensation of a lump in the throat. Unlike gastroesophageal reflux disease (GERD), silent reflux doesn’t typically cause heartburn, but it can still inflict damage on the upper airway. Dietary changes are a cornerstone of treatment for this condition, as certain foods can aggravate or soothe the upper digestive tract. Studies emphasize that low-acid, anti-inflammatory, and alkaline-rich foods can reduce irritation and promote healing of the laryngopharyngeal area. Moreover, a tailored reflux diet helps to reduce the frequency of reflux episodes and improve quality of life for patients.
Understanding Silent Reflux
Silent reflux, medically known as laryngopharyngeal reflux (LPR), is a condition where stomach contents flow backward into the larynx and pharynx without triggering the typical symptom of heartburn. Common symptoms include chronic throat clearing, persistent cough, hoarseness, a sensation of a lump in the throat, and difficulty swallowing. Unlike gastro-esophageal reflux disease (GERD), LPR often presents subtly, making diagnosis more challenging. It is sometimes referred to as “silent” because the usual burning sensation is absent, despite acid-related damage occurring in the throat. (1)
Several factors contribute to the development of silent reflux, including malfunctioning of the upper esophageal sphincter, increased abdominal pressure, obesity, and dietary habits. Stress, smoking, and poor posture may further exacerbate symptoms. Crucially, diet plays a central role in symptom management. Research supports the effectiveness of a plant-based Mediterranean-style diet rich in alkaline and low-acid foods, which has been shown to significantly reduce LPR symptoms. (2) (3) Dietary modification is not just preventive but also therapeutic when integrated with other lifestyle changes. (4)
Best Foods to Eat with Silent Reflux
Silent reflux, or laryngopharyngeal reflux (LPR), often causes throat irritation without heartburn. Choosing the right foods can ease symptoms and promote healing by reducing acid and inflammation naturally.
Alkaline foods help reduce acid exposure in the esophagus, making them beneficial for individuals with silent reflux. A 2017 study compared a plant-based, alkaline diet to proton pump inhibitors and found significant symptom relief. Alkaline-rich diets reduce pepsin activity, a key irritant in reflux, according to NIH research. (5) Further, clinical insights support this dietary approach, emphasizing symptom control. (6) Additionally, nutritional reviews highlight its role in mucosal healing. (7)
2. Low-Acid Fruits and Vegetables (Especially Green and Leafy)
Low-acid produce such as leafy greens and melons reduce esophageal irritation, making them ideal for silent reflux management. A NIH study indicates these foods minimize gastric acid stimulation. (8) Research from JAMA further supports plant-forward diets. ScienceDirect reviews show reduced inflammation with green vegetables. (9) Additional findings underscore their protective effect against laryngopharyngeal reflux. (10)
3. Whole Grains
Whole grains like oats and brown rice provide fiber that supports digestion and minimizes reflux triggers. A NIH study indicates fiber-rich diets reduce gastroesophageal symptoms. (11) ScienceDirect research links whole grains to reduced acidity. JAMA findings confirm their gastrointestinal benefits. (12) Additional clinical reviews recommend them as part of reflux-friendly eating. (13)
4. Lean Proteins
Lean proteins like chicken, turkey, and tofu reduce reflux symptoms by avoiding high fat content, which delays gastric emptying. NIH evidence supports low-fat diets for reflux relief. (14) A JAMA article recommends lean protein intake. Scientific reviews stress protein choice in reflux management. (15) Further research highlights tofu’s protective effects. (16)
5. Healthy Fats in moderation
Healthy fats like those in avocados and olive oil, when consumed in moderation, may soothe the esophagus and aid digestion. NIH findings show monounsaturated fats improve gut motility. (17) ScienceDirect research supports moderated fat intake for reflux control. (18) JAMA insights warn against high-fat diets. Additional reviews recommend plant-based fats for symptom relief. (14)
6. Herbal Teas and Soothin g Beverages
Herbal teas like chamomile and slippery elm provide anti-inflammatory relief and help coat the esophagus, reducing reflux discomfort. NIH research supports herbal remedies for upper GI symptoms. (19) ScienceDirect studies confirm mucosal protective effects. (20) Clinical data shows benefits in reducing pepsin irritation. JAMA articles also discuss natural soothing agents. (21)
7. Dairy Alternatives
Dairy alternatives like almond, oat, and soy milk are gentler on the digestive system and reduce acid reflux symptoms. NIH research confirms lower inflammatory responses with plant-based dairy. (22) ScienceDirect studies show better symptom outcomes. (23) JAMA data links cow’s milk with reflux aggravation. Additional evidence supports soy and almond as effective substitutes. (24)
8. Quinoa and Brown Rice
Quinoa and brown rice are low-acid, whole grains that help reduce esophageal irritation and promote digestion. NIH sources show these grains support gut balance. (25) ScienceDirect reviews highlight their role in reflux prevention. (26) Clinical studies confirm symptom reduction. (27) JAMA insights suggest choosing whole grains over refined to limit acid reflux.
Sample 1-Day Meal Plan for Silent Reflux
A well-balanced meal plan tailored for silent reflux can ease discomfort and prevent flare-ups. This sample 1-day plan includes soothing, low-acid foods that support digestive health and symptom relief.
- Breakfast: Oatmeal with banana and almond milk
- Lunch: Quinoa salad with grilled turkey and steamed broccoli
- Snack: Melon slices with flaxseeds
- Dinner: Baked salmon with sweet potato and sautéed spinach
- Evening: Chamomile tea with a rice cake
Foods and Habits to Avoid
Certain foods and habits can trigger or worsen silent reflux symptoms. Avoiding acidic, spicy, and fatty foods, along with lifestyle changes, is key to managing this condition effectively.
Foods to Avoid
Citrus fruits like oranges, lemons, grapefruits, and their juices are highly acidic (pH 2–3). This acidity can irritate the delicate lining of the throat and esophagus, which is already sensitive due to LPR. These foods lower the pH level of the stomach and esophagus, exacerbating reflux symptoms.
2. Tomatoes and Tomato-Based Products
Tomatoes are naturally acidic and contain malic and citric acid, which can lower the lower esophageal sphincter (LES) tone, allowing acid to escape into the throat. Tomato sauces, salsas, and even ketchup are common culprits for reflux flares.
3. Chocolate
Chocolate contains caffeine, theobromine, and fat, all of which contribute to relaxing the LES. This encourages the backward flow of acid into the throat, increasing irritation and inflammation associated with silent reflux.
4. Peppermint
Though often considered soothing, peppermint can have the opposite effect in reflux sufferers. It relaxes the LES, leading to increased acid reflux episodes. This effect is especially problematic when consumed as tea or flavoring.
5. Fried and Fatty Foods
High-fat meals delay gastric emptying, leading to increased gastric pressure and greater likelihood of reflux. Greasy foods also decrease LES tone, making reflux more frequent and severe.
Habits to Avoid
1. Eating Large Meals
Consuming large portions causes stomach distension, which increases pressure on the LES. This pressure can force acid up into the esophagus and throat. Smaller, more frequent meals help control reflux symptoms.
2. Lying Down After Eating
Gravity plays a vital role in keeping stomach contents down. Lying flat immediately after eating allows acid to move up the esophagus more easily, particularly during digestion. It’s recommended to wait at least 2–3 hours after eating before reclining.
3. Wearing Tight Clothing Around the Abdomen
Tight clothing compresses the stomach, raising intra-abdominal pressure and pushing acid into the esophagus. Wearing loose-fitting clothes can significantly help manage silent reflux symptoms.
4. Eating Late at Night
Late meals don’t allow the stomach enough time to empty before lying down, increasing the likelihood of nocturnal reflux. This is especially problematic for silent reflux, which often worsens during sleep.
Additional Tips for Managing Silent Reflux through Diet
Beyond food choices, managing silent reflux involves mindful eating habits, portion control, and meal timing. These dietary strategies can significantly reduce symptoms and support long-term throat and digestive health.
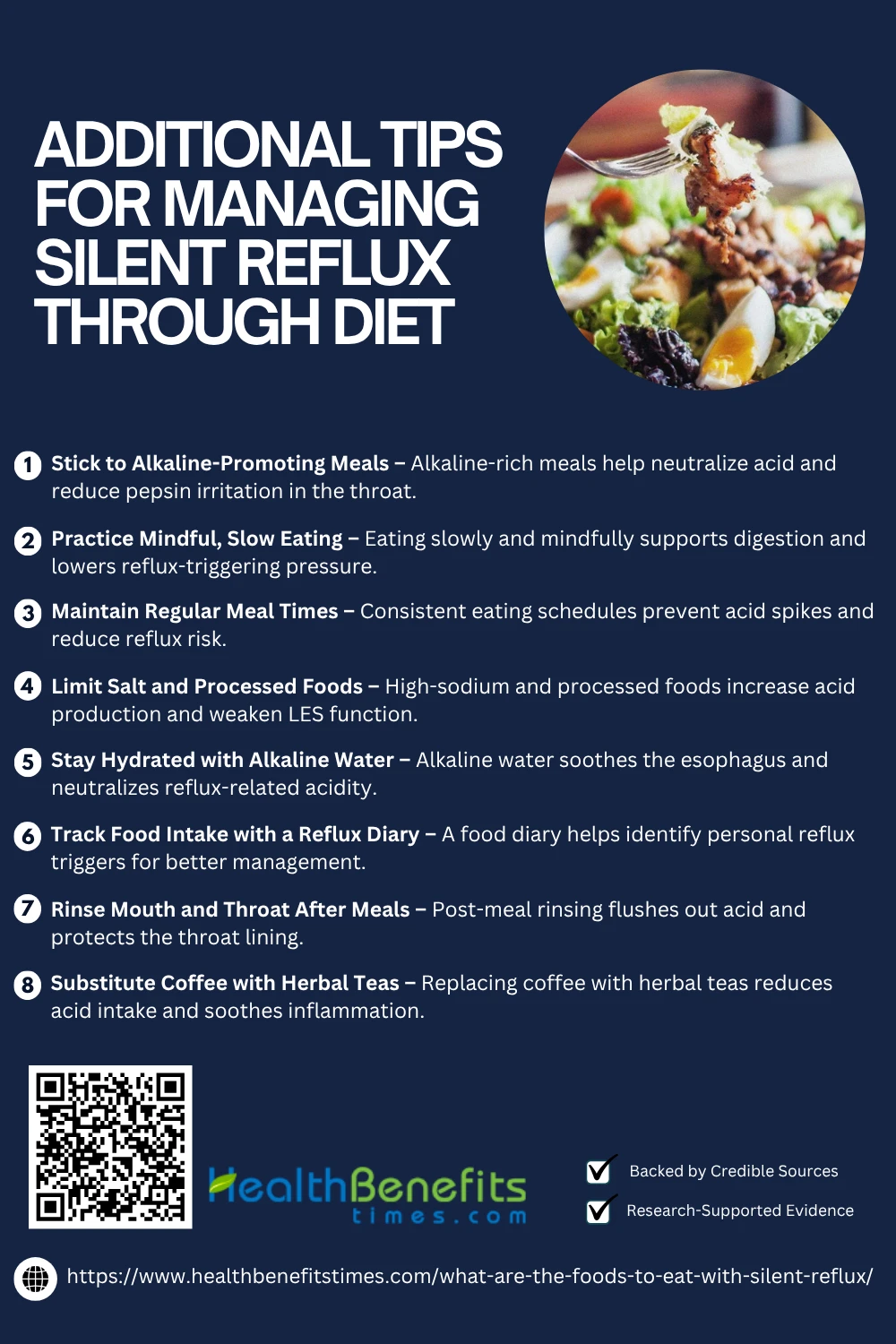 1. Stick to Alkaline-Promoting Meals
1. Stick to Alkaline-Promoting Meals
Incorporating alkaline foods like leafy greens, cucumbers, melons, and root vegetables can help neutralize excess stomach acid and deactivate pepsin, a key irritant in silent reflux. These foods soothe the esophagus and reduce inflammation. A JAMA study demonstrated that a plant-based, alkaline diet was as effective as proton pump inhibitors. Supporting this, NIH data and ScienceDirect reviews confirm their role in reflux symptom control. (7) (18)
2. Practice Mindful, Slow Eating
Eating slowly and chewing thoroughly aids digestion and reduces intra-abdominal pressure, a trigger for LPR. Rapid eating increases air intake, bloating, and the risk of reflux. Mindful eating also promotes better food choices and portion control. An NIH review emphasizes its impact on reflux management. (13) Clinical findings and ScienceDirect data further support slower eating for reducing esophageal irritation. (11) (20)
3. Maintain Regular Meal Times
Keeping consistent meal times stabilizes stomach acid production and prevents late spikes that trigger reflux. Skipping meals or erratic eating schedules can lead to overeating or delayed gastric emptying. ScienceDirect research emphasizes the value of structured eating for gastrointestinal health. (15) NIH sources and JAMA studies link irregular eating patterns with increased LPR symptoms. (25)
4. Limit Salt and Processed Foods
Processed foods and high-sodium meals are linked to increased gastric acid production and weakened LES tone, contributing to reflux. They often include acidic preservatives and saturated fats. A JAMA investigation identified processed meats and snacks as dietary risk factors. NIH analysis and clinical studies recommend avoiding these for improved reflux outcomes. (17) (14)
5. Stay Hydrated with Alkaline Water
Alkaline water (pH > 8) may deactivate pepsin and reduce acidity in the esophagus, offering immediate symptom relief. Frequent small sips throughout the day soothe the throat and dilute acid. A NIH study found alkaline water inactivates pepsin in vitro. (7) ScienceDirect data and JAMA reports support its inclusion in dietary reflux therapy. (20)
6. Track Food Intake with a Reflux Diary
Using a food and symptom diary can help identify personal reflux triggers, which vary widely among individuals. Recording what you eat and when symptoms occur enables better diet planning. A clinical review emphasizes this as a non-invasive, self-monitoring tool. (14) NIH guidance and ScienceDirect reports recommend diaries for effective LPR management. (26) (8)
7. Rinse Mouth and Throat After Meals
Rinsing with warm water, saline, or baking soda after meals helps flush out residual acid and pepsin, protecting the larynx and esophagus. This simple habit reduces ongoing mucosal damage. NIH studies demonstrate its protective effects. (19) ScienceDirect publications and clinical guidelines recommend this especially after acidic meals. (21) (20)
8. Substitute Coffee with Herbal Teas
Coffee is acidic and stimulates gastric acid production. In contrast, herbal teas like chamomile, ginger, or slippery elm have anti-inflammatory and mucosal-soothing properties. A ScienceDirect article notes herbal tea’s benefits for reflux. (20) NIH reviews and JAMA references endorse herbal options for LPR relief. (19)
When to See a Doctor or Dietitian
If silent reflux symptoms—such as chronic throat clearing, hoarseness, or persistent cough—persist for more than a few weeks, it’s crucial to see a doctor for an accurate diagnosis and potential laryngoscopic evaluation. Professional intervention ensures proper treatment and helps rule out more serious conditions like Barrett’s esophagus. (14) Dietitians play a vital role in designing personalized reflux plans, tailoring diets to reduce triggers (JAMA) and enhance mucosal healing. (11) (15) Collaborative care improves outcomes and long-term symptom control. (8)
Conclusion
Managing silent reflux through diet is a practical and effective way to reduce symptoms and improve quality of life. Choosing alkaline, low-acid, and anti-inflammatory foods like leafy greens, whole grains, lean proteins, and soothing herbal teas can help minimize irritation and promote healing. Avoiding common triggers such as spicy, fatty, and acidic foods is equally important. Additionally, adopting healthy eating habits—such as smaller, frequent meals and avoiding late-night eating—can further support digestive health. While dietary changes may not cure silent reflux, they play a crucial role in symptom control. For personalized guidance, consult a healthcare professional or registered dietitian.